
Affordable family practitioner service in the offing
A committee appointed by the Health Care & Nutrition Minister Nimal
Siripala de Silva to examine a new proposal for an affordable family
practitioner service presented by Prof. Herbert Aponso at the Annual
Health Forum in
|
Affordable family practitioner
|
Feb. 2007 is seeking public views on the project.
Dr. Palitha Abeykoon (WHO Advisor to the Ministry of Health) and
Prof. Herbert A. Aponso (Emeritus Professor of Paediatrics) of the
Committee which has finalised its recommendation on the proposal in a
communication to the Health Watch state âAt this stage we are seeking
the views of the public on this proposals and we would appreciate the
publication of the script in the Health Watch.
While thanking the two members for seeking our cooperation to help in
getting the public views, we would appreciate if the Health Watch
readers write to us too briefly their views on this proposal.
The proposal in brief
An affordable family practitioner service
A Public/ Private Enterprise
Presented at the Annual Health Forum (Feb. 2007) by Prof. Herbert A.
Aponso, on behalf of a Committee appointed by the then Director General
of Health Services, Dr. Athula Kahandaliyanage, presently, Secretary,
Ministry of Health Care & Nutrition
The Committee
Chairman Dr. Amal Harsha de Silva, Director, Private Health Sector
Development
Members; Dr. palitha Abeykoon (WHO), Senior Advisor to the Minister
of Health; Prof Herbert A. Aponso, Emeritus Professor of Paediatrics, U,
Peradeniya Prof Lalitha Mendis, Consultant Medical Education, Former
Dean, F/Medicine and former Director, PGIM, U. Colombo; Dr. W. A.
Ferdinand, President, Independent Medical Practitioners Association; Dr.
Preethi Wijegunawardena, President, College of General Practitioners;
Dr. Leela de A. Karunaratne, Retired Founder Professor of Family
Medicine, U. Jâpura
Dr. Sarath Paranavithana, Senior Family Practitioner; Dr. Ruvaiz
Haniffa, Senior Lecturer in Community Medicine, U. Kelaniya
Introduction
A senior politician, well experienced in financial affairs, in a
letter written to the Hon Minister of Health, and distributed by the
DGHS to all members of the committee appointed to examine the proposal
submitted by Prof. Aponso, has said.
âFree Education and Free Health have been two of the greatest social
welfare measures taken in this country for the last 60 years. But the
time has now come for us to take a critical, meaningful and objective
look at both these wonderful things, and improve, amend, and modify them
for the greater good of our country...
|

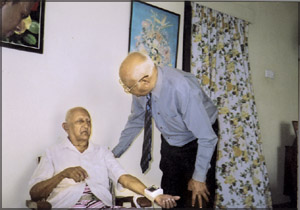
Prof. Herbert A. Aponso
|
Anybody taking a look at our Government Hospitals and their
Outpatient Departments today and also taking into consideration the very
high fees and charges that people have to pay for good medical care and
drugs, should welcome any move to improve the Family Practitioner
Service in our country.
It is most gratifying to note that, in the field of Education,
far-reaching socio-economic measures have been introduced. These include
the Mahapola Scholarships for University students, and for school
children a free mid-day meal and a (reported) annually expenditure of Rs.
2.6 billion for textbooks and school uniforms.
This proposal, in the field of health, is a preliminary step to
âimprove, amend, and modify them for the greater good of our country.â
It has recently been reported that âthe government has allocated Rs.
77 billion for nation building activities, and 32 subjects including
major social and economic development, rehabilitation, and
reconstruction projects.â
Benefits to the State and to the Public
a. The goodwill and support of a large majority of the people in the
stateâs policy of social and health development
b. The provision of a comprehensive primary health care service, by
oneâs own doctor, in all parts of the country, including the rural areas
that the presently undeserved, in contrast to primary curative service.
This would prevent disease and promote good health considerably, and
consequently, in the long-term, reduce the incidence of disease at
Primary, Secondary and Tertiary levels.
c. The prevention of the practice of âquacksâ who are causing much
damage to unsuspecting patients.
In this connection, it should be mentioned that Legislation is being
introduced to make it mandatory for all doctors in the private sector to
display prominently their qualifications (with the country of the
medical school), Registration Number of the SLMC, and Hours of
Consultation.
d. Reducing medical expenses by making only an affordable payment for
establishment expenses. If a Family Practitioner is available close by,
as is being suggested, there would be a considerable saving in terms of
time, cost of travel, and incidental expenses, when visiting a hospital
OPD, a person often spends about Rs. 50 to Rs. 100.
e. There shall be no privatization of the health services - On the
other hand, there would continue to exist an entirely free and less
congested state OPD service to those who are unable to make the
establishment payment, and the payment of the low-cost medicines that
are being suggested, or to those who prefer the OPD service for any
other reason
f. Provision of incentives and benefits to doctors so that they would
opt for Family Practice as their chosen career; family practice, which
is the cornerstone of primary health care, âis fast dying out in our
country,â
The Proposal
The main focus is on government intervention to reduce the cost of
primary health care, and the provision of self-employment opportunities
to doctors
Central Organisation
In the first instance, it would be necessary to set up an
organisation such as a Family Practitioner Committee (FPC), and later if
reckoned necessary a Corporation, for the following purposes: general
organisation, decisions on recruitment and remuneration of doctors and
ancillary staff and on special incentives/benefits for the doctors who
would opt for Family Practice as their chosen career, establishment of
pilot projects and later the permanent stations, and to monitor,
evaluate the system and deal with all problems. It would be necessary to
appoint sub-committees for each of these activities. (vide annexures 1
and 2 for two such activities)
Professional requirements of a Family Practitioner (in addition to
the basic medical qualification)
Those recruited for the proposed FP service should possess a training
and experience in Family Medicine. The Diploma in Family Medicine (DFM),
or its equivalent should be made mandatory at a later stage
The training should include aspects of professional and ethical
conduct. It is further suggested that all medical colleges should be
encouraged and supported to provide a training in Family Medicine.
Group Family Practices
Group practices of 4 FPs are recommended, reasons being:
a. to provide a round-the-clock service
b. to facilitate home visits
c. to facilitate doctors to attend medical meetings
d. to reduce the establishment expenses
Only doctors approved by the organisation would be eligible to
practice at these clinics
Clinic Staff
For the purpose of efficient management, the FPs should recruit,
train, an control the necessary ancillary staff, through the FPC would
make the payments through, and on the recommendation of, the FPs.
Preventive Services
It is suggested that each FP should conduct Regular Special Family
Clinics which would include areas such as Antenatal & Postnatal care,
Family Planning services, Child Welfare (including Immunisations),
Screening for the Non-Communicable Diseases (eg, Diabetes, Hypertension,
Atherosclerosis), Health and Nutrition Education, etc.
Drugs and Investigations
FPC should facilitate the establishment of people friendly
pharmacies, such as State Pharmaceutical (SPC) outlets, at every Group
Practice, FPC clinic patients shall be provided free medical
investigations at a state institute, at the request of the FP.
A distinct advantage of this scheme is that the FPs (of the FPC),
would be motivated to prescribe drugs and request investigations
according to an accepted uniform system, thereby avoiding unnecessary
investigations and expensive drugs.
The ultimate goal would be for the FPC to have a laboratory and
pharmacy for each group practice, these may be established in
collaboration with the SPC.
Records
Accurate medical information is essential for, the prevention of
unnecessary repetition of investigations and drugs, information on drug
history, continuity of health care, referrals, etc.
In this connection, computer facilities are recommended. FPs should
be appointed as Registrars of Births and Deaths, when vacancies occur,
this would provide more reliable records, which are necessary for Health
Planning.
Expenses by the public (for this service)
A basic principle of this public/ private enterprise is that it is
obligatory for the users of this service to make an affordable payment,
as âthutu panduruâ, to cover a part of the establishment expenses;
suggestion, Rs. 40. In this connection, it should be noted that the
government OPDs would still be available to those who wish to seek
treatment there.
Financial Provision and Remuneration for FPs
The present private full-time and part-time general practitioners
There would be no interference with their practices.
There is provision for part-time practitioners in the State sector to
collaborate with this scheme in various ways, such as:
a. Secondment for service while preserving all the privileges of the
state sector employment.
b. Joining this scheme, with the option of reverting back to the
State sector, after a period of 5 years, without losing any of the
service benefits of employment in the State sector.
c. Doing âlocumsâ in this scheme, while being in the State sector
employment
Pilot projects
It would be necessary to start a few pilot projects initially; 5
pilot projects carried out for one year would cost about 30 m (vide
annexure 2).
Financial Provision for the proposed plan for a Family Practitioner
(FP) Service
Recommendations of a sub-committee. Prof Herbert A. Aponso, Dr. Nimal
Sanderatne (Former Deputy Governor, Central Bank of Sri Lanka, and
Chairman, Bank of Ceylon), and Dr. Ranil Abayasekara (Senior Lecturer in
Economics, University of Peradeniya)
Preamble
In recent times public/ private enterprises have been initiated and
supported by the State in order to provide an enhanced cost-benefit to
the public.
The introduction of a hospital charge at the Sri Jayawardenapura
Hospital, which provides a relatively better service than at other
government hospitals, can be considered to be the beginning of this
policy change in the health sector.
Thus the suggestion to levy an affordable payment for establishment
expenses, for a better service, is not a new concept, it is not a
radical change in health policy.
The Main Expenses
These can be categorised as:
a. Initial capital expenditure for buildings, equipment, etc.b.
Recurrent expenses for the central administration, and rentals for
electricity, etc
c. Payment to doctors and clinic staff The salaries of the clinic
staff, are calculated as the mean of the initial and the retiring
salaries.
Provision is being made for the payment of 15% for either a Provident
Fund or Pension scheme. Provision is also made for locum FPs.
Initial Capital Expenditure
The initial capital expenses for equipment, including computers for a
4 FP group practice would amount to about Rs. 500,000.
It is probably a fair assumption that funding for this non-recurrent
expenditure would be available from international organisations or local
supporters. Therefore this capital expenditure is not taken into account
in calculating the financial provision. It is expected that the State
would provide suitable accommodation for the Group Practices, as it
would have to do so in any expansion of the health service.
The father of Geriatrics
Eight years ago in an article titled âAgeing: On a full sea we are
afloatâ contributed by me to an English daily (âThe Islandâ 22nd.
February 1999) it was stated that âalthough an American, Dr. Ignatz
Nascher, invented the word geriatrics, the English invented the
speciality because geriatrics is one medical speciality where Britain
has led the wayâ.
It is, therefore, interesting to read in a recent issue of the
British Medical Journal (BMJ, 9 June 2007, volume 334) of how Ignatz Leo
Nascher came to be called the father of geriatrics.
Although, geriatrics has a long and fascinating history, many believe
that the field entered the modern era with the publication in 1914 of
Ignatz Leo Natscherâs bookâ Geriatrics : The Diseases of Old Age and
their Treatmentâ. This bookâs origins are interesting in that it began
with a ward round.
As a medical student in New York Nasher was part of a team that came
to an acutely ill woman, whose condition Nascherâs professor described
in words that can be still heard today,â Old ageâ.
When this young student asked what could be done to help the patient,
he was shocked by his teacherâs response: âNothing!â. Several years
later Nascher wrote this book, in which he first formulated the term
âgeriatricsâ from the Greek âgeronâ (old man) and âiatrokasâ (medical
treatment).
The head of geriatrics, Soroko Hospital, Ben Gurion University of the
Negev, Beer-Sheva, Israel, in reviewing this book, has this to say; âThe
book makes for fascinating reading. Much material, especially that on
therapeutics, is of course dated.
However, the clinical approach described, and above all, the spirit
of hope expressed in the book, are as relevant today as were almost a
century ago.
Just as we have learnt the paediatric patient is not merely a little
adult, Nascherâs book shows us that the older patient is in many ways
very different from the middle aged person she once was. This book is a
testimony to this pioneerâs dedication and an appropriate rejoinder to
his pessimistic professor of medicineâ.
- Dr. Terernce PERERA
WHO steps into save Asian traditional medicines from piracy
Dr. Viraj PERAMUNA
Traditional medical practitioners (TMP) in Sri Lanka will be glad to
hear that the World Health Organisation (WHO) is taking steps to
safeguard the traditional medicines and medical practices in the
developing world from being pirated by interested groups in the world
using Intellectual Property rights.
In a paper on âTraditional Medicine Strategy for 2002-2005â the World
Health Organisation say:
The World Health Organisation estimates that traditional systems of
medicine serve the health needs of about 80 per cent of the worldâs
population and the goal of health for all can never be achieved without
traditional medicines.
Practices of traditional medicine (TM) vary greatly from country to
country and region to region, as they are influenced by factors such as
culture, history, climatic conditions, personal attitudes, ideology and
philosophy.
However, there has been renewed and wider interest in TM not only in
the developing countries but also in the developed countries (especially
herbal medicine) for many obvious and hidden reasons.
For millions of poor patients in the vast rural areas of developing
and under developed countries, the use of TM is the only affordable and
accessible source of primary health care. Studies reveal that there are
more TM providers than the allopathic providers especially in the rural
areas.
The increased use of TM in the developed countries is mainly due to
the adverse effects of chemical drugs, questioning of the approaches and
assumptions of allopathic medicine, greater public access to information
on traditional medicine.
Long historical use of many practices of TM including experience
passed from generation to generation, has demonstrated the safety and
efficacy of the above.
Despite its existence and continuous use over many centuries and its
popularity especially during the last decade, TM has not been
effectively recognised by the Ministries of Health in most countries.
Consequently, education, training and research in this area have not
been accorded due attention and support.
The World Health Organisation (WHO) launched its âTraditional
Medicine Strategy for 2002-2005â to enable TM to play a far greater role
in reducing excess mortality and morbidity, especially among
impoverished communities incorporating four objectives; policy, safety,
efficacy, quality, access and rational use.
The paper also emphasises that intellectual property rights issues
should be taken into consideration as many developing countries have a
wealth of indigenous TM knowledge and/or natural and generic resources
used in TM practices.
If not, it will pave way to losing their indigenous knowledge,
ownership and right to use TM to âbio piracyâ within the worldwide trend
and the complex legal arrangements of IPR, which are not well-known to
the owners of community knowledge and generic resources.
In conclusion, the paper presents some guidelines to policy and
action to promote and encourage TM. Following are some of these
guidelines;
* National governments should encourage discussions among traditional
healers, health professionals and the general public to formulate and
develop public policies including regulations, which address the
utilisation of traditional medicines in primary healthcare.
* International organisations, governments, NGOs, manufacturers and
traditional healers are to develop ethical criteria for the promotion of
traditional medicines and herbal remedies.
* Academic and research institutes, traditional healers, NGOs and
community organisations should be supported by national governments to
raise public awareness of the benefits and risks of traditional
medicines and herbal remedies.
Lankan doctor honoured with the Man of the Year Award
The American Biographical Institute USA has nominated Dr. Terence
Perera to be a recipient of this yearâs Man
|

Dr. Terence Perera
|
of the Year Commemorative Gold Medal. It is the wish of the
Institute to confer on a small number of men, representing a variety of
countries this medal in recognition of contributions made to society.
Dr. Perera served for over 12 years as WHO Senior Advisor in Maternal
and Child Health for the South East Asia Region. Prior to that, he was a
Consultant Paediatrician in the Ministry of Health, Sri Lanka and was
among the pioneers in the field of paediatrics in this country.
He was appointed consultant paediatrician to the General Hospital
Anuradhapura in 1962, the first paediatric post for the North Central
Province.
Here, as the Chairman to the Committee on Rehabilitation of Disabled
Children, he initiated a programme for Education of Disabled Children in
Regular Schools, for the province.
In the area of control of infectious diseases and immunization, he
was helpful in evolving a scheme for data recording of infectious
diseases and immunization in children in paediatric wards in hospitals
and child welfare centres in the community.
His active involvement in pioneering work in Oral Rehydration Therapy
(ORT) in this country is documented by WHO, including the opening of the
first Oral Rehydration Centre at the General hospital, Kalutara in the
1960s as the Consultant paediatrician. ORT is now recognised as a top
medical advance that has saved several million lives of children in
developing countries, dying from diarrhoea and dehydration.
He was also instrumental in initiating an outreach premature baby
service, in collaboration with the then Institute of Hygiene, Kalutara,
to follow up the infants after their return home from hospital.
Later, he served as the fist Director of the National Integrated
Programme of Maternal and Child Health and Family Planning. At one time,
he was the Visiting Professor of International Maternal and Child
Health, to the University of California, Berkely, and to the State
University of San Diego.
On return to the country, after retirement from the international
civil service, he got himself involved in community service working with
the underprivileged shanty dwellers in partnership with Rev. Fr. Michael
Catalano, a Jesuit priest, the founder of the Shanti Community Animation
Movement (Shanti CAM), which is now over 30 years. |

