|
dailynews |
|
|
|
|
|
OTHER LINKS |

|

|

|
|
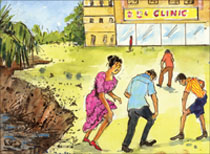
Chikungunya (The bending up) sickness:It's not the Bird FluKUMUDINI Ranawake (Lecturer Dept. of Zoology) of the Kelaniya University writing to us on the current mosquito borne Chikungunya viral infection which is spreading in Sri Lanka too, says that some people have the mistaken belief that it is 'Bird flu' but studies have proved that it is not. The special feature of this infection is characterised by fever, body aches and pains lasting for two weeks and in some cases even up to three weeks, is that it causes the affected to go about in a stooped position on bended knees. The very word Chickungunya means - bended stooped.
Do you know that Chikungunya has arrived in the United States? "Colorado, Louisiana, Maryland, Minnesota and at least half-dozen other States have reported cases of travellers returning from visits to Asia and East Africa sick with the mosquito-borne virus, according to the U.S. Centers for Disease Control and Prevention", stated The Star Ledger, a US newspaper last week. It also pointed out that France has reported 850 cases of travel-associated Chikungunya, the United Kingdom 93 and the United States at least a dozen, according to the CDC. Other Chikungunya infected travellers have been diagnosed in Belgium, French Guyana, Hong Kong, Italy, Kenya, Malaysia, Martinique, Norway, Switzerland and Sri Lanka. Therefore it is going to be a threat in any place, any country where vector populations exist. Hot topic cases confirmedIn Sri Lanka, it is still a hot topic and suspected cases were mainly reported from Mannar, Kalmunai, Trincomalee and a very few from Western and the Southern part of the country. MMU of the Faculty of Medicine, University of Kelaniya has confirmed the disease using few blood samples taken from the clinically suspected patients earlier this month. Sensing the outbreaks in India, we can be never sure of avoiding outbreaks here, with the favourable conditions for vector breeding opens along with the rainy season. Therefore it is essential to put a step forward and join hands together towards the controlling of Chikungunya vectors, mainly Aedes aegypti. Nothing to do with Avian FluInitially general public had a misleading thought that Chikungunya has something to do with avian Flu, may be due to the way it sounds. But it is very true that Chikungunya has nothing to do with Avian Flu at all. The name Chikungunya was derived from the Makonde word meaning 'that which bends up' regarding the stooped posture developed as a result of arthritic symptoms of the disease, referred to as poly-arthralgia in medicine. Chikungunya was first recorded in Tanzania, Africa in 1952. A feverish infectious disease outbreak among the Makonde people (Makonde - an ethnic group) on the Makonde Plateau in Tanzania was studied by Marion Robinson and W.H.R. Lumsdon and they isolated the virus and described the disease as Chikungunya in 1955. The Chikungunya virus or so called CHIKV belongs to the Genus - Alphavirus and Family-Togaviridae. And the viral group is indicated as Group IV ((++)ssRNA). Therefore it is a RNA virus so as for Dengue. Chikungunya is transmitted mainly by the mosquito Aedes aegyhpti but recent findings (Pasteur Institute, France) suggests that A.albopictus also can transmit the disease as the virus has suffered a mutation enabling it to be transmitted by A.albopictus. In India A.aegypti is recorded as the major vector and the virus is maintained in the human population by a human-mosquito-human transmission cycle. But in Africa, the virus is reported to be transmitted initially through a sylvatic transmission cycle where wild primates and mosquitoes of different Aedes species such as A.luteocephalus, A.furcifer and A.taylori take part in. According to WHO Chikungunya fever displays interesting epidemiological profiles. Major epidemics appear and disappear cyclically, usually with an inter-epidemic period of 7-8 years, but sometimes as long as 20 years. As for India, the current outbreaks threatening to be an epidemic is after 32 years. After Chikungunya was first recorded in Africa there were several outbreaks all over Africa. But the most recent one was recorded during 1999-2000 in Kinshasa, in the Democratic Republic of the Congo. 50,000 people were estimated to be infected there. The first Asian outbreak was in Thailand in 1958. Since then in various South East and East Asian countries suffered from several outbreaks. And the most recent outbreak other than the current Indian one was in Java Indonesia in 2001-2003 striking after a 20 year gap. WHO records prevail that in Sri Lanka the virus strains were recorded in 1969. An interesting studyAn interesting study done by some scientists of the National Institute of Virology, Pune, India (Published in the online journal emerging Infectious Diseases of the Centers for Disease Control and Prevention (CDC), United States) has revealed some important facts on the current outbreak of Chikungunya in India. According to them the earlier outbreaks (from 1963-1973) were due to the Asian genotype of CHIKV. But the current isolates from the few localized cases belong to the Central/East African genotype. They also have identified that this genotype had been introduced less than 5 years before the current outbreaks after grouping Central/East African genotype with Yawat isolate. (In this study they have used blood samples from 1938 suspected case patients from three States, Andhra Pradesh, Karnataka and Maharashtra). According to a research done by some French scientists (Published in the online journal, PLoS Med; July 2006) they have pointed out that Indian Ocean Chikungunya outbreaks are caused by the genomic macroevolution of CHIKV. Their findings revealed that there is a specific change in the position 226 of E1 protein referring to the isolates, obtained from patients in November and December 2005, displaying a Val at this position instead of Ala. Although position 226 is relatively variable among alphaviruses, it was observed that a single mutation at this position (Pro to Ser) allowed SFV (Semliki Forest virus) to adapt to growth in cholesterol-depleted insect cells. As SFV is a close relative of CHIKV scientists argue that the change in the position 226 of CHIKV enables it to grow successfully in cholesterol-depleted mosquito cells. (Viruses normally require cholesterol in the host cells to infect those, but mosquitoes usually do not have sufficient amount of cholesterol in their cells for viruses to infect them efficiently). Most probably Sri Lanka is having the same Central/East African genotype but no one can make conclusions without proving it. Therefore it is up to the molecular biologists to work on this issue as the virus is becoming more unpredictable and more virulent according to the current investigations. The incubation period can be 2-12 days but it is usually 3-7 days. Acute Chikungunya fever typically lasts a few days to a couple of weeks. But the joint pain may lasts for weeks or months. Chikungunya is not a life threatening illness and it is thought to confer life long immunity. As the vector is same for both Chikungunya and dengue co-occurrence of the diseases is also evident. In that case, it is so important to distinguish between two accurately with the aid of laboratory diagnosis. Though Chikungunya is not life threatening dengue in severe forms (DHF or DSS) can be lethal. No vaccine or specific antiviral treatment for Chikungunya is available. Symptomatic treatment for mitigating pain and fever using anti-inflammatory drugs along with rest usually suffices. Paracetamol may relieve fever and aching. Aspirin should be avoided. As no vaccine is available prevention is entirely dependent upon taking steps to avoid mosquito bites and elimination of mosquito breeding sites. Followings are WHO instructions for Prevention and Control of Chikungunya. To avoid mosquito bites: Wear full sleeve clothes and long dresses to cover the limbs; Use mosquito coils, repellents and electric vapour mats during the daytime; Use mosquito nets - to protect babies, old people and others, who may rest during the day. The effectiveness of such nets can be improved by treating them with permethrin (pyrethroid insecticide). Curtains (cloth or bamboo) can also be treated with insecticide and hung at windows or doorways, to repel or kill mosquitos. To prevent mosquito breedingThe Aedes mosquitoes that transmit Chikungunya breed in a wide variety of manmade containers which are common around human dwellings. These containers collect rainwater and include discarded tires, flowerpots, old oil drums, animal water troughs, water storage vessels, and plastic food containers. These breeding sites can be eliminated by draining water from coolers, tanks, barrels, drums and buckets, etc; Emptying coolers when not in use; Removing from the house all objects, e.g. plant saucers, etc. which have water collected in them, Co-operating with the public health authorities in anti-mosquito measures. Role of public health authoritiesNational programme for prevention and control of vector borne diseases should be strengthened and efficiently implemented with multisectoral coordination, Legislations for elimination of domestic/peridomestic mosquitogenic sites should be effectively enforced, communities must be made aware of the disease and their active cooperation in prevention and control measures elicited. High Blood Pressure: The disease without symptomsProf. M. R. Mohideen President Sri Lanka Hypertension Society (SLHS) speaking at a symposium held on Hypertension at the Lional Memorial Auditorium at Wijerama Mawatha in Colombo said that high blood pressure which is affecting about one fourth of the world population today does not produce any symptoms and is often detected during routine medical consultations. He went on to say; Hypertension is perhaps the commonest risk factor for the commonest cause of deaths in adults; cardiovascular disease. It is estimated that currently nearly 7.2 per cent of worldwide deaths are attributed to high blood pressure. Nearly one fourths of the world population has high blood pressure.
By 2020, hypertension will be the most common risk factor for death and disability in the world. In Sri Lanka too, hypertension has emerged as an important health condition. It is estimated for recent surveys that nearly one in five persons in the 30-65 year age group has high blood pressure. This amounts to over a million persons affected by this condition. It is projected that patients with high blood pressure seeking treatment in hospitalization will increase by 40 per cent by 2010 compared to the present rates. High blood pressure is one of several risk factors for coronary heart disease, stroke and kidney disease. If blood pressure is well controlled, development of these complications is largely avoidable. However, good control of blood pressure of those undergoing treatment has been disappointingly low. A recent study in Sri Lanka has shown that only 22 per cent of those with high blood pressure have satisfactory levels of control. High blood pressure does not produce any symptoms and is often detected during routine medical consultations. A heart attack and stroke are often the first instance that high blood pressure is detected. Increasing age, weight, salt intake and alcohol use contribute to high blood pressure in the community. The Sri Lanka Hypertension Society (SLHS) which was formed in 2003 has been involved in a number of activities which included the development of guidelines for doctors in the treatment of hypertension. The SLHS hopes to widen the scope of its activities with a programme that will improve awareness and knowledge of high blood pressure among the public. Screening for hypertension among the public, training paramedical personnel in blood pressure measurement, updating the knowledge of doctors are some of the other activities that will be undertaken in the coming year by the SLHS. By 2020, HBP will be the most common risk factor for death and disability. Genetech and Sri Jayawardhanapura researchers identify and isolate Chikungunya virus from patientsDr. Neil Fernandopulle, Senior Scientist/Head Genetic Molecular Diagnostics writes: Last week researchers from the Molecular Medicine Unit at the University of Kelaniya used the Polymerase Chain Reaction test (PCR) and found evidence of Chikungunya virus in some patient's samples. Further studies done by researchers from Genetech Research Institute and the University of Sri Jayawardhanapura have led to the isolation and culturing of the virus from suspected cases. The team tested blood from 12 suspected cases (provided by the Epidemiology Unit) and detected the presence of the virus in 4 of the samples and cultured the virus from one sample. The identity of the cultured virus was confirmed by using Chikungunya antibodies provided by Professor Robert Tesh from the WHO arbovirus reference center at the University of Texas Medical Branch in Galveston. The research team consisted of Dr. Faiz Marikar, Dr. Nalaka Kanakaratne, Dhammika Seneviratne and Dinali Ranaweera (Genetech), Chinthika Gunaskera (SJP), Dharshana Naula (SJP), Mallika Peelawatte (SJP) and Dr. Aravinda de Silva (SJP and Genetech). Chikungunya virus was first described in Africa in the 1950s. Subsequently the virus has caused epidemics in many countries in Asia including Sri Lanka, which experienced a large epidemic in the 1960s. The current epidemic in Sri Lanka is probably related to large epidemics of Chikungunya reported from several Indian Ocean islands last year. Subsequently, the virus moved into mainland India and caused large epidemics in several states. Researchers at Genetech are currently doing studies to understand how the Sri Lankan virus is related to the Chikungunya viruses responsible for recent epidemics in this region. People at risk for dengue are also at risk for Chikungunya as the same mosquito vector transmits both diseases. In fact, it is not easy to distinguish the two diseases using clinical findings alone. Genetech currently offers PCR based diagnostic tests for both dengue and Chikungunya, and are in the process of developing a combined diagnostic test which can detect both viruses at once. The PCR test for Chikungunya can only be performed on specimens collected during early stages of the disease (people within the first 4 days after the onset of fever). Clotted blood samples can be used to detect the virus, and test results can be provided within 24 hours. |